
The 5 Types of Vaginal Pelvic Organ Prolapse
Pelvic organ prolapse (POP) most often occurs in individuals with a vagina/middle opening, but it can also occur in individuals with a penis. For this article, we will focus our discussion on those with a vagina, which includes natal women, transgender women who have undergone genital reconstruction surgery, and trans men who have a middle genital opening.
Pelvic organ prolapse occurs when the muscles and connective tissue (fascia, ligaments, and tendons) of the pelvic floor become weak and loose. This allows the pelvic organs to move downwards within the pelvis and into the vaginal canal.
The statistics vary on how many individuals suffer from pelvic organ prolapse, ranging from 3% of women in the United States to 50% of women over 50. But one resounding sentiment is clear: Pelvic organ prolapse is something that is not talked about, screened for, or treated as often as it should be. Therefore, those who experience it may be unnecessarily suffering in silence. Let’s take a look at what pelvic organ prolapse is and what you can do about it.
There are many subtypes within the broad umbrella term of pelvic organ prolapse. Your treatment options are based on the type, grade, and symptoms of prolapse.
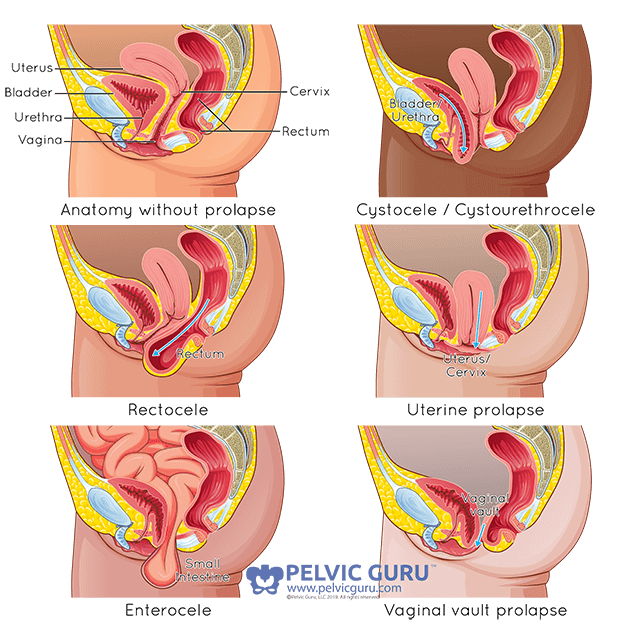
Types of Pelvic Organ Prolapse
The following are types of vaginal/middle opening prolapse.
Cystocele: a cystocele can also be called an anterior prolapse or bladder prolapse. It happens when the front wall of the vagina/middle opening slackens, allowing the bladder to move into the vaginal/middle opening canal.
Cystourethrocele: A cystourethrocele happens when both your bladder and your urethra move into the vaginal/middle opening canal. Some providers may separate these, calling them a cystocele and a urethrocele.
Rectocele: A rectocele, also called posterior prolapse, is when the back wall of the vagina/middle opening relaxes and allows for the rectum to move into the vagina/middle openingl canal.
Uterine Prolapse: A uterine prolapse happens when the uterus moves into the vaginal/middle opening canal.
Enterocele: An enterocele happens when the small intestine moves into the vaginal/middle opening canal.
Vaginal Vault Prolapse: A vaginal vault prolapse occurs when the uppermost part of the vagina/middle opening sags and loses its shape, moving down into the vaginal/middle opening canal.
***It is important to note that nothing is truly entering your vagina/middle opening in the sense that it breaks through your skin. It simply means that the wall of the vagina/middle opening loosens and the organ on the other side presses into that space. Sort of like if you grasp your shirt and push your thumb into it. You don’t break through your shirt, but you can move your finger into the free space on the other side.
Symptoms of Pelvic Organ Prolapse
If you have the following symptoms or feelings, you may have a pelvic organ prolapse.
Talk to your health care provider or physical therapist if you:
- Have a heaviness or dullness in your abdomen or canal
- Have a sense that there is something coming into or falling out of your canal
- See or feel something in or coming out of your canal
- Have pain with intercourse
- Have difficulty with bowel movements, including having to place your finger in the vagina/middle opening or push around the rectum to complete a bowel movement.
- Have difficulty with urination, including:
- Urinary frequency
- Incontinence
- Hesitancy
- Incomplete bladder emptying
How Pelvic Organ Prolapse is Diagnosed
You can check to see if you have a prolapse at home.
To do this, you can squat over a mirror or stand with your foot up on the side of the tub. Then cough or bear down. This pressure causes your organs to move down. When you do this, you may notice downward motion. If you see downward motion, pay attention to how far that motion occurs. This shows you the level, or grade, of your prolapse. For more on grading a prolapse, see below.
Even if you see prolapse, it is not something that should cause you too much concern or worry. Like all medical conditions, your condition is determined by both a physical examination and a discussion of your symptoms.
During a pelvic examination, your provider will ask you to cough or bear down to create increased pressure in your abdominal canister, or your belly. When you do this, they look at your vaginal opening/middle opening to see if any of the above prolapses occur.
If they do observe a prolapse, they can associate a grade to the degree the organs move down with your efforts. The pelvic organ prolapse grading system is as follows:
0 = No prolapse noted
1 = Prolapse occurs just inside the vaginal opening/middle opening
2 = Prolapse pushes against the vaginal opening/middle opening
3 = Prolapse moves outside of the vaginal opening//middle opening
4 = Prolapse moves completely out of the vagina/middle opening
Treatment Options for Pelvic Organ Prolapse
The treatments for prolapse vary depending on the grade of your prolapse and your symptoms. If you have a few symptoms that affect your daily life, you may be able to reduce symptoms with exercise and lifestyle changes. However, if your prolapse is a high grade or your symptoms really affect your daily life, you may need to have prolapse repair surgery.
BUT before we worry about whether or not you need surgery, let’s focus on what you can do RIGHT NOW… pelvic floor physical therapy! Pelvic floor physical therapy can help you address all those negative symptoms listed above. And the crazy thing is, it isn’t all about kegeling (aka tightening your pelvic floor muscles)! There are lots of other exercises and many benefits of doing pelvic floor physical therapy with a certified physical therapist.
Physical therapy may work on:
- Strengthening your hips
- Managing your bowels
- Ergonomics with lifting
- Coordination of your abdominal and pelvic muscles
- Activity modification
And those are just a few things a physical therapist can help you with. I think one of the most important things I offer to people are ways they can manage their symptoms at home. You can do physical therapy exercises in the comfort of your own home.
If you feel that would benefit from pelvic floor physical therapy or think you are experiencing symptoms that may require diagnosis, you can book a FREE 20-minute consultation HERE.
Or, if you’d like to learn more about all things pelvic floor health, head over to Instagram! You can always reach out in the DM’s if you have any questions!
More content you may like:
Some of the links on this page may be affiliate links. Laura Meihofer’s LLC is a participant in the Amazon Associates Program and others, as an affiliate advertising program designed to provide a means for sites to earn advertising fees by linking to products Laura organically uses and trusts. If you purchase a product through an affiliate link, your cost will be the same, but Laura will automatically receive a small commission. Your support is greatly appreciated and helps her spread her message!








Sorry, the comment form is closed at this time.